|
Suki Series C | Deloitte Wearables
December 8, 2021
|
|
|

|
|
Together with
|

|
|
|
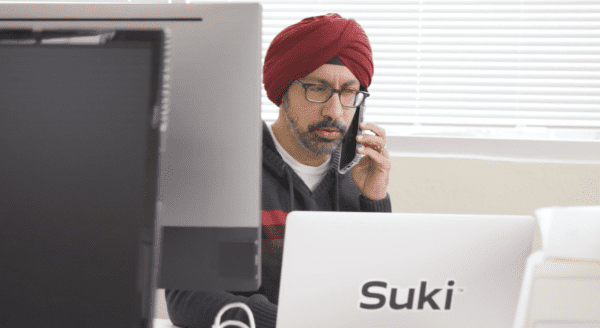
“We are at a turning point in healthcare, where it’s now imperative to offer technology that improves physician burnout caused by documentation and administrative burden.”
|
|
Suki CEO Punit Soni
|
|
|
|
Although some physicians might love the time-consuming administrative tasks that help make a successful patient visit, Suki recently raised a $55M Series C round to help develop AI-enabled voice tools for those that don’t.
As of the latest funding, the company has raised a total of $95M to support the development of Suki Assistant, its voice-first digital assistant, and Suki Speech Service, its platform designed to improve the accuracy and experience of voice solutions.
- Suki uses natural language processing to create patient notes and streamline administrative tasks, such as retrieving information from the EHR or ICD-10 coding.
- The digital assistant supports doctors “in any clinical setting, as well as any specialty,” and can be configured with personalized commands to adapt to unique workflows.
- Early research shows that the assistant lowers average time per note by 76%, while decreasing claim denials by 19% through the creation of detailed documentation.
- Voice is quickly entering the healthcare spotlight, with Notable raising a $100M Series B in September and Microsoft acquiring Nuance for nearly $20B earlier this year.
The Takeaway
The accuracy of voice recognition has crossed a threshold that allows it to be effective in a growing number of consumer products, as well as in healthcare. These tools can now understand a speaker’s intent regardless of most accents or phrasing, leading to wider adoption within previously difficult use cases.
In a roundabout way, Suki is taking a tech-heavy approach to making technology less visible, removing it from between the doctor and the patient so that more attention can be given to providing clinical care. Taking advantage of voice is a natural way to accomplish this, giving Suki a good shot at reducing burnout by allowing more time for physicians to actually practice medicine.
|




|
|

|
|
Companies continue to develop new features for wearables that blur the line between consumer products and medical devices, a trend that Deloitte predicts will be a dominant theme in 2022.
A new report from the consulting firm predicts that more healthcare improvements are on the horizon for wearables, which might increase their effectiveness in the clinical setting as early as next year.
- Smartwatches that measure blood oxygen saturation (SpO2) will likely become more common, as low SpO2 is a potentially life-threatening symptom that’s hard to detect unassisted.
- Continuous blood pressure monitoring could improve due to advances in photoplethysmography (PPG), Raman spectroscopy, and infrared spectrophotometers.
- Over 10% of smartwatch owners are now using them to detect COVID-19 symptoms, with 15% of smartwatch owners purchasing them after the onset of the pandemic.
Although Deloitte projects total wearables shipments to climb from 320M units in 2022 to 440 units in 2024, it also notes several headwinds that could slow adoption.
- Interoperability is cited as a top priority for provider adoption of new technologies, yet only 10% have integrated data from wearables into their EHR.
- Data privacy remains a concern for 40% of smartwatch owners, a figure that rises to 60% among those who use smartwatches exclusively to track their health.
- Increased regulatory scrutiny is anticipated as smartwatch outputs are integrated into EHRs, with most current devices avoiding HIPAA by collecting data for personal use.
Deloitte does not view these obstacles as insurmountable, and believes that simultaneous advances in sensors, semiconductors, and AI will lead to further innovation. Both big tech and the medical community see a bright future for wearables, and their continued investment could make it “a self-fulfilling prophecy.”
|




|
|
Nuance’s Patient Engagement Must-Haves
Consumer demands are shifting, and they’re looking to get more out of their digital health technology. Nuance outlines the 5 must-haves for your patient engagement strategy here.
|
|
- Polychronic Management: Lyn Health recently emerged from stealth to create a new care model for the 34M US adults estimated to be “polychronic.” Lyn aims to support patients managing multiple chronic conditions by combining virtual primary care, medication management, and behavioral health support in a single point-of-contact. The model collaborates with employers, health plans, and providers to augment current programs in a way that better coordinates care and drives value for all stakeholders.
- Virtual CBT Effectiveness: A study published in JMIR investigated the effectiveness of virtual cognitive behavioral therapy (vCBT) on 30 patients with chronic pain, finding that the integration of vCBT into standard pain care was associated with a significant improvement in pain interference with daily activity, but had no effect on pain intensity. The researchers point out that vCBT could lower care expenses for treating pain interference, but a larger sample size is needed to verify the findings.
- Robo-Nurses: Cedars-Sinai Medical Center has two new staff members designed to reduce nurses’ daily workloads: identical twin robots named Moxi (here’s a video of them in action). The mobile robots assist with tasks such as delivering lab samples and collecting medications from the pharmacy, reportedly saving clinical teams over 300 miles of walking since the pilot program began in September.
- Financial Experiences Matter: A new survey of 1,500 adults by Cedar (no relation to Moxi’s parents) found that 93% of respondents list the quality of their financial experience as an important factor in deciding whether they’ll return to a healthcare provider. Over 25% of respondents have left a negative provider review due to unexpected expenses, which is likely tied to the 31% of patients who aren’t satisfied with the coordination between their healthcare provider and payor.
- EMRs Should Be Like Spotify: A recent article by former athenahealth founder and current Zus Health CEO Jonathan Bush explored the evolution and “death” of the EMR, making the case that static record keeping is due to be usurped by a more dynamic solution. Bush draws an analogy to Spotify, stating that providers are ready to dispense with keeping an “out-of-date, memory-hogging copy of just their own songs” and are instead ready for a “database of all the songs in the world.” The logic is that the latter solution is better, and as he puts it, “we know how to do this shit.”
- COVID’s Telehealth Impact: An American Medical Association (AMA) report revealed that telehealth accounted for 5% of Medicare’s physician services spending in 2020, peaking at a 16% share in April before leveling out at 6% towards the end of the year. Prior to the pandemic, telehealth accounted for only 0.1% of the Medicare total, but the AMA anticipates sustained levels of telehealth usage for the foreseeable future.
- Fertility Funding: Femtech startup Proov recently closed $9.7M in Series A funding to help create and distribute at-home diagnostic tests for reproductive health. Proov created the first FDA-cleared PdG-testing kit to help women confirm ovulation and gain better insight into their fertility window, supported by an app that assists with tracking results and adhering to care protocols.
- Pandemic Racial Disparities: New research from Komodo Health found that while overall hospital admissions for acute myocardial infarction declined during the pandemic, they declined only 2% among patients of color, versus 11% among White patients. The findings add to the evidence that care was deferred during the pandemic, and highlights the ongoing disparities for people of color, which Komodo attributes to factors such as more frequent COVID-19 infections and lack of access to preventive care services.
- Quartet + InnovaTel: Quartet Health had a busy week, which started with raising a $60M funding round ($222M total funding) and ended with the acquisition of InnovaTel Telepsychiatry. Both moves are geared towards advancing Quartet Health’s new strategic direction centered around helping patients quickly obtain mental health care during times of need.
- Telehealth Growth Rebounds: Fair Health’s Monthly Telehealth Regional Tracker showed that national telehealth use climbed by over 2% in September to 4.4%, the second consecutive month of growth following a sustained streak of declines earlier this year. Although the uptick in telehealth usage can be attributed to the spread of the delta variant throughout the month, COVID-19 was not among the top five telehealth diagnoses, which remain largely concentrated on mental health conditions.
|
|
|
|
|